|
• Diabetes Leader Editions |
|
• Educational Videos |
|
• Philippine Clinical Practice Guidelines for Diabetes |
|
• Article of the Month |
ARTICLE OF THE MONTH
DIABETES AND AGING
Contributed by: Myla D. Capellan, M.D.,FPCP,FPSEDM

“To care for those who once cared for us is one of the highest honors.“
We are not immortals, we cannot be forever young. In the coming days we will just be surprised our love ones are aging. Our folks who once cared for us now needs our help.
Patients in the elderly population are defined as people more than 65 years of age and above. It is the phase in our lives wherein our bodily system can experience slow, progressive impairment in function that continues until the end of life.
Why do we have to be extra careful in taking care of our elderly diabetic patients? Elderly diabetics are prone to complications of diabetes especially if they have long-standing illness. In addition to complications of diabetes, because of failing bodily functions they usually have many medications to take (polypharmacy), functional disabilities, cognitive impairment, depression, urinary incontinence, falls, and malnutrition. The management of these population should be individualized taking into account the different diseases that they have aside from diabetes.
In frail diabetic patients, avoidance of low blood sugar, low blood pressure and possible interaction of the different medications they are taking as compared to younger diabetics.
Here are some highlights to share in treating our elderly patients
-
Blood sugar goals:
-
Avoiding hypoglycemia:
-
Reducing Cardiovascular Complications:
-
Lifestyle Modification:
-
Special Needs of Elderly with Diabetes:
-
Screening and Treatment of depression, these prevalent in this age group because some live alone. Just simple questions to ask: “Do you feel sad?” or “Do you feel you have been losing interest or feeling down in the past month?” If the answers are positive, we can address this problem to a specialist.
-
Enhancement of social and family support through building rapport with relatives and care givers at home.
-
Adaptation for cognitive or mental changes. Sometimes we have to limit information, frequent repetition and short sentences. We can also combine verbal and written instructions. Giving time to fully understand what was said.
-
Reducing fall risks, which is high in elderly with diabetes due to the following :
-
Peripheral Neuropathy (sensory and motor pain)
-
Altered foot structure (Charcot’s foot)
-
Muscle Weakness (decreased strength)
-
Orthostatic hypertension
-
Decreased Vision
-
Risk of hypo or hyperglycemia
-
Osteoporosis
-
Vision
-
Pneumonia and flu vaccinations
For older patients, we should target our goals with less hypoglycemia (low sugar levels), we have to consider that some of them doesn’t have much appetite or they have other accompanying illnesses other than diabetes (kidney failure, heart ailment, Alzheimer’s, stroke, cancer patients undergoing chemo and radiotherapy). They also have erratic eating patterns. Doctors should be informed of these conditions so he can treat the patient accordingly.
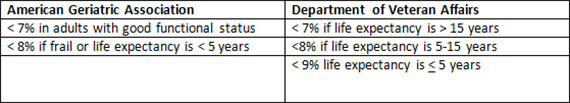
The glycosylated hemoglobin (HbA1c) levels, a measure of your three months average sugar levels and sugar levels were targeted to as follows:
- A1c goal should be < 8% (from the usual 6.5 or 7 %) in frail, medication-treated older adults with multiple functional problems and life expectancy is less than 10 years. Fasting and before meals blood sugars should be between 160 and 170 mg/dl (8.9 to 9.4 mmol/l)
- For fit older patients, A1c goal should be < 7.5% should be considered in medication-treated patients. Fasting and before meals blood sugars should be between 140 and 150 mg/dl ( 7.8 to 8.3 mmol/l).
- Individualized targets for the very old may be even higher at < 8.5% and we should include all efforts to preserve the quality of life and avoid hypoglycemia (low sugar levels) and other related complications. An A1c of 8.5 percent is estimated average glucose of 200 mg/dl (11.1 mmol/l).
Older adults are very prone low sugar levels specially if they are very frail. Most common complaints from our patients are decreasing appetite, with many medications they are taking they are full already, erratic food intake (forgetting they missed their meals) and other conditions aside from diabetes. Older patients have lesser complaints of low sugar symptoms like tremors, sweating, hunger pangs. They usually manifests as dizziness, weakness, confusion and delirium which make reporting of low sugar levels delayed.
Low sugar levels in older populations may lead to grave heart conditions (i.e. heart attack). Very low sugar levels will require hospitalization, sometimes older patients have a long time recovering from a very low sugar levels and may lead to dementia if it occurs more often.
Avoidance of low sugar levels in older adults is one of the most important deciding factor in choosing medications for them. Relatives should note these symptoms and if there are changes in the eating pattern of their patients. Notify their doctor of this occurrence. It is advised to monitor blood sugars of elderly patients specially if they are on insulin and sulfonylureas which are the most of frequent medication to cause low sugar. It is also highly advised that someone will look after older patients taking and preparing their medications because they might make a mistake of taking it twice and might cause their sugars to drop.
Both diabetes and age are major risk factors of having heart disease. Coronary Heart disease is the leading cause of death in older patients with diabetes. They said that having diabetes is equivalent to having a heart disease also. There were numerous trials proving that keeping sugars in control and also your cholesterol levels can prevent one from having a heart disease. Cholesterol lowering medications is a staple in a diabetic patient. Treating hypertension with antihypertensive agents is recommended. We recommend ACE or ACE inhibitors as their first line antihypertensive except if there are contraindications to it (coughing, kidney failure). Aspirin is recommended for high risk patient.
Change in the way we live is the cornerstone in the prevention of complications of diabetes. Exercise is beneficial to maintain physical function, reduce cardiac risk, improves insulin sensitivity and advantage of reducing arthritic pain, increasing quality of life and prevention of falls. Smoking cessation can decrease risk of cardiovascular complication. Medical Nutrition Therapy is a process of nutrition prescription tailored for diabetic patients. It is a very important aspect in the management of diabetes. Diet can greatly lower our patient’s glycemic control. We have to consider that elderly patients have altered taste perception, coexisting illnesses, dietary restrictions, dentition problem, gastrointestinal malfunction, memory decline leading to skipped meals. Obese elderly may benefit from caloric restriction and exercise to target weight loss of 5% body weight. Likewise, older adults at risk for undernutrition should be guided by a nutritionist regarding their diet.
Aside from medical management, they have special needs that we need to look at to and these are as follows:
There are many aspects of care we should give to our elderly diabetic patients, the more they need our guidance to treat them. We have to monitor them closely because they don’t complain often and they try to hide it from us. Caring for our elderly diabetics has its complexities, but with thorough caring, we can easily identify their problems and render solutions that can give them comfort. Family support and good communication with caregivers, doctors and nurses will make their lives easier.
Sources:
-
Standards Of Care. American Diabetes Association. 2016
-
Hammounda et al. Optimizing Diabetes Control in Geriatric Patients. Journal of Diabetes Research and Clinical Metaboilism. 2012
-
International Diabetes Federation. Managing older people with type 2 diabetes. Global Guideline. Feb 2014
-
Mennely et al. Diabetes in the elderly. Can J Diabetes 37 (2013) S184-S190